Katie's Legacy
The First Couple of Days
At 6:52PM on Monday May 19, 2008, Katherine Alexa Manning was born in Milford Hospital (CT). Katie was a very healthy 6 pounds 14 ounces and 21″ long. As you can imagine, she was immediately the center of attention for her first time parents. The abundant happiness that Katie brought to our world was spectacular. She epitomized perfection- angelic glow, soft skin, and a visible innocence that brought all who were lucky enough to meet her to their respective knees. In short, she was Mommy and Daddy’s little munchkin.
After a whirlwind Monday night and a perfect Tuesday, Katie was all set to be discharged on Wednesday morning. Unfortunately, she never quite made it home that day. Due to an alarming drop in oxygen levels Katie was transported to Yale New Haven Hospital. After an exhausting day of tests, Katie was diagnosed with a congenital heart defect known as Hypoplastic Left Heart Syndrome(HLHS). HLHS is a rare and potentially fatal condition that is addressed by 3 palliative open heart surgeries.
At just 4 days old, Katie underwent her first operation (the Norwood Procedure) and although it was referred to by the surgeons as “the most difficult surgery they have to complete” she came through the ordeal better than anyone anticipated. In fact, after a series of expected ups and downs, she was home within 3 weeks.
The Middle
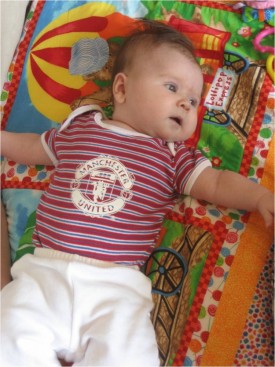
The next few months were uneventful by HLHS standards. Katie was taking a series of medications, had weekly doctors' appointments, and required a level of attention that was far beyond that of your average newborn, but we were happy and grateful for every day we got to spend with our Munchkin. From June through mid-August Katie lived as close to a normal baby’s life as possible. However, a routine heart catheterization in late August to rectify a coarctation of Katie’s aorta led to a dissection of her aorta wall and a series of events nobody anticipated. After failing to fix the coarctation at the first attempt, the cardiology team performed another “cath” two weeks later, but did not execute the procedure due to fears that the dissection would worsen from their efforts. After consulting experts from around the nation, it was deemed safe to proceed with a stent placement to fix Katie’s coarctation. During her third cath, which took place only 3 weeks after her first, the medical team successfully placed the stent to correct Katie’s coarctation. Unfortunately, the procedure caused Katie to go into cardiac arrest, creating neurological damage to Munchkin.
During late September and early October the focus was taken away from HLHS and instead the medical staff tirelessly worked on improving Katie’s neurological state. Remarkably, Katie went from no responsiveness following the cardiac arrest to an almost complete return to her normal behavior within a month. Prior to her series of caths, Katie was a precocious baby, active, and engaging. Her decline was heart-wrenching, but her rapid return was inspirational. Unfortunately, the resurgence was short lived. Just as Katie began to make significant strides neurologically her heart problems again resurfaced. In mid October, a fourth heart catheterization completed as a pre-operative exploration before her 2nd surgery (The Glenn Procedure) showed that Katie’s heart function was significantly diminished. This meant that she was in need of her next surgery sooner than expected. However, the cath also yielded another cardiac arrest, albeit minor compared to her first episode.
The Last Weeks
Katie had her 2nd open heart surgery on October 29th 2008 (the Glenn Procedure). It was a long and arduous procedure that saw the surgeons perform the Glenn procedure twice, kept Katie on by-pass for over 2 hours, and resulted with Katie’s condition being defined as “marginal.” From her first surgery in May to her second surgery 5 months later there was an obvious and dramatic shift in Katie’s long term prognosis. Confidence was replaced by hopes and prayers.
On November 5th, while Katie was supposed to be recovering from her surgery a week earlier, her condition truly started to spiral out of control. Swelling to her upper torso coupled with plummeting numbers had the doctors very concerned. Within hours the plan went from “let’s watch and see” to “let’s get to the cath lab” to “we need to get her to the O.R. immediately.” . This emergency effort included Katie’s third Glenn, but also her 3rd cardiac arrest. Unfortunately, her issues didn’t end there. Katie’s swelling was caused by severe clotting that dramatically compounded her condition. She returned to her room in a “very, very, marginal” condition, so much so that the entire surgical team stayed in the hospital that night. The doctors bluntly stated: “she may not make it through the night.” That was Wednesday.
Thursday brought a day of respite but little improvement in Katie’s condition. She was stable but not improving. On Friday, the surgical team scheduled a “wash-out” to clean up from Wednesday's emergency surgery…it sounded so routine. This course of action began with 2 or 3 medical staff and ended with a team of more than 12 doctors and nurses crowded into Katie’s room in the ICU performing yet another open heart surgery. She began to clot again and her condition was too precarious to risk moving her to the O.R. Her parents sat outside the window to Katie’s room as a medical team saved her life, yet again. When they emerged, her parents sensed the change in their tone and body language. Katie’s medical condition was now far removed from her initial HLHS battle. Katie was now battling HLHS, neurological insult, and an inexplicable blood clotting condition. After the dust settled, Katie's parents met with the cardiology and surgical team where they were informed that there was nothing more the team could do for Katie.
At 5:22pm, on November 9th, 2008, Katie breathed her last breath as she lay in her mother’s arms. Munchkin was at peace.
To read more about Katie’s life, visit www.katiemanning.wordpress.com